The Importance of Post‑Operative Rehabilitation After a Frenotomy
As a General Practitioner on the Gold Coast performing oral tie releases (frenotomies), I regularly help families optimise breastfeeding, speech potential, and overall oral function for their infants. A common question from parents is: “Do we really need to do the post‑release stretches?” Let’s take a closer look at why these exercises are so important for long‑term results.
1. Preventing Re‑Attachment and Repeat Surgery
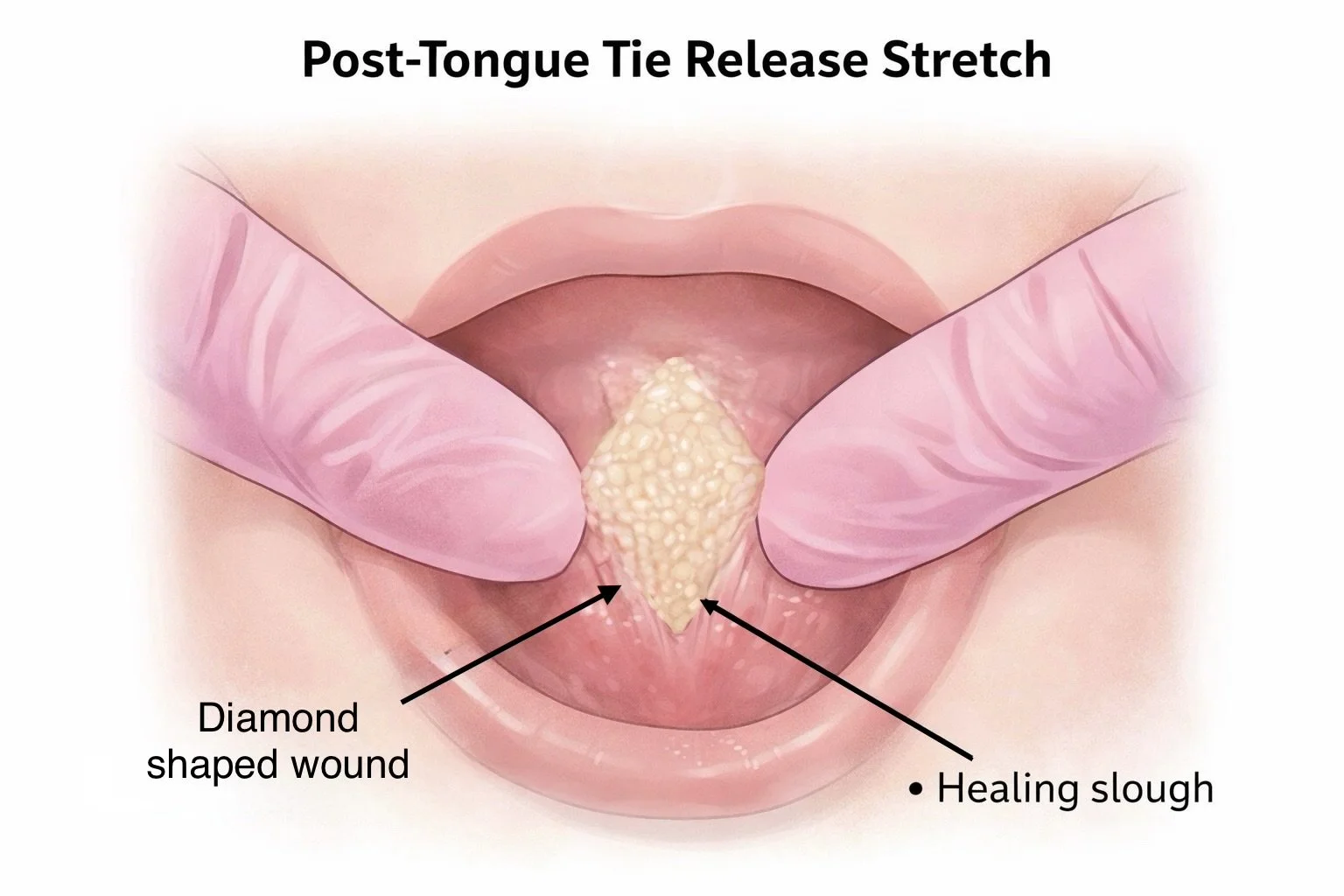
Although research remains limited, available studies consistently show that babies whose families perform regular post‑operative stretches have lower rates of frenulum re‑attachment and fewer repeat releases. Stretches keep the healing wound mobile and separated while new tissue forms, allowing the tongue to heal freely and functionally.
2. Minimising Scarring
Post‑release stretches limit scar formation by gently counteracting the body’s natural wound contraction. This helps the new frenulum remodel into a soft, flexible band rather than a short, tight scar.
After a frenotomy, the wound quickly fills with granulation tissue and collagen, which peaks around days 14 -21. During this phase the healing “diamond” can feel firmer or smaller - a normal part of the process. Without gentle stretching, collagen fibres tighten and shorten, mimicking a recurrent tie.
Regular lifts and tongue stretches:
Lengthen collagen fibres during healing, allowing a more elastic scar.
Prevent early adhesions that cause true re‑attachment.
Maintain the tongue’s range of motion (elevation, protrusion, lateralisation).
As I often explain to parents: “If you never move a knee after surgery, it stiffens and scars; controlled stretching keeps it moving and stops the scar from locking it down.”
3. Improving Feeding and Functional Outcomes
Evidence suggests that babies who complete structured stretching programs experience fewer ongoing feeding difficulties, less scar tissue, and greater comfort during feeding. Stretches are not just about keeping the wound open - they support proper tongue function, suck strength, and coordination.
Adjunct therapies such as infant myofunctional therapy or gentle bodywork further enhance functional outcomes beyond surgery alone.
4. Restoring Tongue Movement and “Muscle Memory”
While the frenectomy releases the physical restriction, the tongue’s movement patterns and muscle memory often need retraining. Studies and case reports (e.g., Dodal et al., 2024) show that targeted tongue exercises after release improve muscle awareness, posture, and mobility far more effectively than surgery alone.
Combining frenectomy with professional myofunctional or physiotherapeutic guidance helps ensure the tongue learns its new range of motion and maintains those gains.
Timing Matters
Stretches are usually started within 24 - 48 hours after the procedure, while the wound is still soft and pliable. The most critical period is between days 5 and 21, when the scar tissue naturally tries to contract. Consistent daily stretches through this phase help prevent restriction and promote optimal healing.
Recommended Support Practitioners
I recommend parents begin gentle rehabilitation immediately after release, alongside early follow‑up with an experienced chiropractor, physiotherapist, osteopath, myofunctional therapist, or lactation consultant. These professionals can demonstrate the correct technique for lifts, stretches, and oral motor exercises, giving parents confidence at home.
Here on the Gold Coast, I work closely with trusted infant specialists to provide multidisciplinary rehabilitation. Ideally, families arrange a pre‑surgery consultation with their chosen provider to plan post‑operative bodywork and feeding support in advance - ensuring calm, coordinated care from day one.
Clinical Take‑Home
The body naturally pulls wounds together; stretches remind healing tissue to stay longer and looser.
Consistency during the first 3 - 4 weeks is crucial - this is when the tissue wants to tighten most.
Gentle, regular movement helps new tissue form into a flexible, functional frenulum rather than a restrictive scar.
For Gold Coast Parents
If you suspect your baby has an oral tie, speak with your local lactation consultant, physiotherapist, myofunctional therapist, chiropractor, or osteopath. If feeding or movement challenges persist despite conservative care, you can arrange a thorough assessment and release with me for evidence‑based, family‑centred treatment and thriving results.
References
Dodal AA et al. (2024). Postoperative Tongue Exercises for Ankyloglossia Following Lingual Frenectomy. Cureus, 16(9): e69806. PubMed link
Tecco S et al. (2015). Frenulectomy of the tongue and the influence of rehabilitation exercises on the sEMG activity of masticatory muscles. J Electromyogr Kinesiol, 25(4):619–628. PubMed link
Valle‑Del Barrio B et al. (2025). Readhesion of Tongue‑Tie Following Neonatal Frenotomy: Incidence and Impact of Post‑operative Exercises in a Prospective Observational Study. Children (Basel) 12(8):971. PMC link
Navigating Christmas with a newborn on the Gold Coast: Routines, Overwhelm, Circumcision and Tongue Tie
Welcoming a newborn just as the Christmas season ramps up can feel magical and completely exhausting at the same time. The usual newborn chaos is suddenly layered with visitors, travel, noise, and the pressure to “make memories,” which can leave many parents feeling overwhelmed. This is also a time when families may be trying to organise important newborn appointments, check-ups, follow ups, immunisations, weight reviews, midwife appointments, lactation consultant reviews, physiotherapist appointments, ultrasounds, circumcisions or tongue tie assessments, all while providers have their own holiday schedules and closures on the Gold Coast.
Why Christmas Feels So Overwhelming
The festive season changes the usual rhythm of day-to-day life, which can unsettle even the most easy-going baby. Newborns thrive on predictability, and Christmas is anything but predictable. Loud gatherings, passing the baby around, late nights, and travel between houses can all contribute to overstimulation and unsettled behaviour.
Common signs a newborn is overstimulated include:
Short, broken naps and difficulty settling despite clear tired signs.
More frequent crying, pulling off the breast or bottle, and fussing at feeds.
Glazed or wide eyes, crying when passed between multiple people, and needing longer to calm once distressed.
Being aware that this is a predictable pattern around Christmas can help reduce guilt. It is not a reflection of parenting ability; it reflects a tiny nervous system being asked to cope with a lot of change all at once.
Protecting Newborn Routines During Festivities
The goal over Christmas is not to maintain a perfect schedule but to protect a few anchors in your newborn’s day. Think of these as the non‑negotiables that help your baby feel secure even when everything else looks different:
Keeping a consistent bedtime “wind‑down” routine (dim lights, nappy change, feed, cuddle, then bed) even if the actual bedtime is slightly later.
Protecting at least one or two good quality naps each day in a calmer, darker space away from the main family activity.
Limiting the number of people holding the baby when they are already fussy or tired, and offering regular “quiet room” breaks.
If you are travelling around the Gold Coast or between relatives’ homes, try to recreate a simple portable sleep environment: a safe sleep space, a swaddle or sleeping bag your baby recognises, white noise if you use it, and the same pre‑sleep cues you use at home. Small consistent rituals can go a long way in a very stimulating environment.
Planning Around Holidays on the Gold Coast
One of the biggest stressors for new parents is trying to coordinate care when many clinics and services adjust their hours over Christmas. This can be particularly challenging for families wanting timely newborn circumcision or are struggling with feeding and want an oral tie assessment for a possible tongue tie and release. Clinics, GPs, lactation consultants and hospitals all have different public holiday arrangements, and some reduce their procedural lists or close entirely for a period.
To reduce last‑minute panic, consider:
Asking about holiday hours for your preferred provider.
Book any non‑urgent newborn appointments (such as routine checks or non‑urgent reviews) a little earlier than you normally might in December, as appointments can book out quickly.
Clarifying who to contact if your usual provider is away: is there a shared on‑call arrangement, a specific after‑hours service, or a local hospital you should attend if worried?
If you will be visiting the Gold Coast from interstate or overseas, it is helpful to research local medical services in advance. Look up GPs who see young babies - having names and numbers saved before you arrive can take an enormous weight off your mind.
Circumcision Timing and Christmas
Many families prefer newborn circumcision to be done within the first weeks of life, but Christmas and New Year can complicate this timing if services are reduced. It can be stressful to realise a preferred time frame overlaps with provider holidays, especially if you have cultural, religious or personal reasons for wishing to proceed within a certain age window.
A few points to consider when planning circumcision around the festive season:
Ask about procedural cut‑off ages and whether these are flexible: some clinics are comfortable up to a certain age or weight, others prefer a more limited newborn window.
Discuss pain relief options, aftercare, and what support is available if you have concerns once you are back at home or travelling between relatives.
Factor in the recovery environment: a quieter couple of days after the procedure is ideal, which may mean saying no to large outings or asking family to visit you at home rather than heading out to busy venues.
If the exact timing you hoped for is not possible because of public holidays, a conversation with your experienced circumcision Doctor, can help you weigh up options, safety and realistic age alternatives. The priority is that the procedure is performed safely, in an appropriate setting, with clear aftercare and an accessible follow‑up plan.
Tongue Tie, Feeding and Festive Disruption
Christmas often coincides with the period when feeding issues become more obvious. Some parents notice latch problems, nipple pain, slow weight gain or unsettled feeding patterns and begin to wonder about tongue tie. At the same time, it may be harder to access face‑to‑face lactation consultants or tongue tie‑experienced practitioners because of holiday closures.
If you are concerned about tongue tie over the Christmas period:
Start by noting specific symptoms: nipple trauma, clicking during feeds, prolonged feeds, poor weight gain, or a baby who seems constantly hungry but never satisfied.
If your usual GP or lactation consultant is away, make a list of local services on the Gold Coast that assess feeding and oral function, including GPs, IBCLCs and dentists or doctors who perform releases.
Use any telehealth options available for initial assessment and triage; sometimes interim feeding strategies can be implemented while waiting for a face‑to‑face appointment.
A frenotomy (tongue tie release) itself is usually quick, but planning matters. You will want to ensure there is support for feeding immediately afterwards and that you can access help if you are worried later that day or in the days following. Arranging this outside the busiest public holiday dates, where possible, can make the whole experience less stressful.
Simple Holiday Planning Timeline
Not every family will have the luxury of long‑term planning, but if you do know Christmas is likely to fall within your newborn period, a loose timeline can help. Think of it as a flexible guide, not another pressure.
8–12 weeks before Christmas (or in late pregnancy if baby is due near December):
Discuss with your GP your preferences around circumcision or tongue tie assessment and ask about holiday hours.
Identify local Gold Coast providers you might use, including after‑hours options for urgent concerns.
2–4 weeks before Christmas:
Confirm any booked procedures or postnatal checks and ensure you understand how to contact someone if you have concerns afterwards.
Prepare a basic “routine‑friendly” plan with your partner or support people: who will act as the gatekeeper for visitors, and how you will handle long days of social events.
During Christmas week:
Prioritise baby’s sleep and feeding cues over social expectations as much as possible.
Be prepared to say no to extra activities if your newborn has had a particularly unsettled day, or if you are recovering from a recent procedure such as circumcision or tongue tie release.
Managing Overstimulation: Practical Tools
Even with the best planning, most newborns will have at least some unsettled days around Christmas. Having a simple, repeatable calming strategy makes it easier to respond when things feel out of control. A basic “calm kit” might include:
A dim, quiet room where you can retreat with your baby for feeds and naps away from the noise.
Swaddles or sleeping bags you use consistently at home, to give familiar touch and smell cues.
White noise, a soft hum, or gentle shushing to help block out household sound.
For visitors and family, set gentle boundaries early. Let people know you may step out with the baby to feed or settle, and that you may limit how much the baby is passed around. Framing it as supporting the baby’s developing nervous system, not rejecting their enthusiasm, can help everyone stay on the same page.
Gold Coast–Specific Considerations and When to Seek Help
For families planning circumcision or tongue tie procedures on the Gold Coast, consider asking:
Whether there is a post‑procedure contact number over the public holidays.
Whether a follow‑up review is recommended, and if so, when and how this will be arranged in the context of holiday closures.
Trust your instincts. If you are worried about your baby’s feeding, hydration, breathing or level of alertness, it is always appropriate to seek urgent care, regardless of the date on the calendar.
Talking to Family About Your Plans
Many parents feel torn between wanting to protect their newborn’s routine and feeling pressure to attend every event or “share” the baby generously with loved ones. Having a clear plan and language in mind can make these conversations easier.
Some phrases that can help:
“We’re keeping things a bit quieter this year so [baby] can cope with all the changes.”
“We may duck out early if [baby] is overtired; we’re still working out their rhythm.”
“We have some follow‑up care booked after the circumcision/tongue tie procedure, so we’ll be staying close to home for a couple of days.”
Most families are relieved when expectations are clearly set and will often adjust happily once they understand that this is about supporting the baby’s wellbeing, not rejecting family tradition.
Bringing It All Together
Christmas with a newborn on the Gold Coast will never be perfectly tidy, but it can be gentler and more manageable with a bit of forward thinking. Protecting a few key routines, planning ahead for circumcision and tongue tie appointments, and understanding how local holiday schedules work all reduce the risk of last‑minute panic. Most importantly, you are allowed to prioritise your baby’s needs and your own recovery over social expectations, even at Christmas.
If you are expecting a baby around the festive season and would like to discuss newborn circumcision or tongue tie assessment and release on the Gold Coast, consider booking a consultation early so that timing, support and holiday plans can be tailored to your family’s situation.
Teamwork at the Heart of Tongue Tie Care: Why Collaboration Leads to Better Outcomes
“Teamwork makes the dream work” - and nowhere is that truer than in managing oral ties. Effective assessment and treatment rely on collaboration between skilled professionals, ensuring families receive comprehensive care and the best possible outcomes. A strong multidisciplinary team - including lactation consultants, bodywork therapists, and experienced doctors or dentists - guides parents through every stage of the journey, from assessment to release and recovery.
As a GP with a special interest in oral ties, dedicated to their diagnosis and management, the importance of teamwork is clear every day in practice. If you suspect a tongue or lip tie, or if a health professional mentions a possible restriction - no matter how minor it seems - seek a proper assessment. Feeding challenges or signs of oral restriction always warrant expert evaluation.
The IBCLC: Feeding and Latch Expertise
International Board-Certified Lactation Consultants (IBCLCs) are the cornerstone of early assessment. They identify and manage feeding difficulties, observing latch quality, milk transfer, and tongue function. Their expertise helps rule out non-tie issues, support parents with practical feeding techniques, and guide care both before and after a release. Ongoing follow-up from an IBCLC ensures that progress is supported and sustainable.
Bodyworkers: Optimising Function and Recovery
Chiropractors, osteopaths, and physiotherapists play a crucial role in addressing other potential causes of feeding difficulties and restriction, as well as the physical effects of oral restriction. By releasing tension in the neck, jaw, and oral muscles, bodywork improves feeding comfort, supports healing, and enhances function post-release. Their whole-body approach complements the procedural aspects of care, especially in babies with significant postural or muscular tightness.
Doctors and Dentists: Skilled Releases Matter
The actual release of the tongue tie, often called a frenotomy or frenectomy, should be performed by a practitioner with experience in paediatric oral ties, such as a doctor or dentist who regularly works with infants and collaborates with a multi-disciplinary team. Experience and exposure to a wide range of cases are more important than titles; practitioners who regularly treat tongue ties can provide safer, more effective outcomes and the good ones will consult closely with IBCLCs and bodywork experts when needed, for this holistic care.
Parents: The Key to Ongoing Success
Parental involvement is the backbone of effective tongue tie management. Ongoing aftercare, exercises, follow-ups and sometimes feeding retraining, require time and commitment, but the results - a smoother feeding journey, improved function, and happier parent-child bonding - are worth it.
When in Doubt, Seek Experience and Second Opinions
Even among professionals, tongue tie cases can be complex. If advice or recommendations don’t feel right, seek a second opinion from an experienced provider. Every baby’s anatomy and needs differ, so finding a trusted team that feels like the right fit is vital. Practitioners with broad experience in oral ties are best placed to offer safe, individualized care.
For families on the Gold Coast seeking tongue tie care, look for teams that work collaboratively across disciplines, with proven experience and strong community recommendations. With the right guidance, even a challenging start can become a positive journey - helping your baby feed, grow, and thrive.
Tongue Tie Care Pathway
Gold Coast GP Answers: Foreskin Retraction in Children & When Is Circumcision Needed?
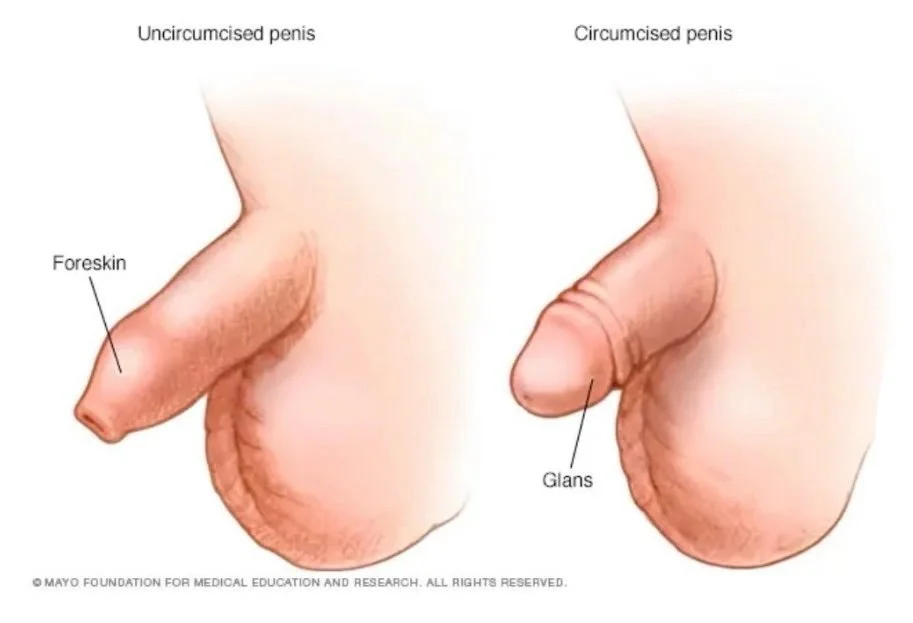
As a Gold Coast GP with a special interest in paediatric circumcision, I’m often asked: At what age should a boy be able to retract his foreskin, and when does it become a problem? This is an important topic not just for parents weighing circumcision, but for all families interested in ensuring healthy development and understanding their options for penis care and circumcision on the Gold Coast.
Foreskin Retraction: What’s Normal?
Most boys cannot fully retract their foreskin at birth, and this is completely normal. Retraction develops slowly and varies dramatically between boys, with only 10% of boys able to retract by age one. Around half can do so by age 10, and 99%, able to retract by age 18. Occasional ballooning of the foreskin during urination, preputial adhesions, or partial retraction in young boys is common and usually not a cause for concern. Infancy and early childhood are not the time to force retraction: gentle cleaning is all that’s required, and full retraction typically comes naturally as boys get older.
When Is Foreskin Retraction a Problem?
Foreskin retraction becomes a problem if it is associated with:
Pain
Recurrent infections
Difficulty urinating
Scarring
Hygiene difficulties
Paraphimosis, (foreskin stuck behind the head of the penis)
Phimosis, (tightening causing physical symptoms).
As a clinician focused on paediatric circumcision and child health, I recommend seeking advice if there are any of these symptoms.
Understanding Your Options: Not Just Circumcision
The main treatment options for foreskin issues include conservative measures, topical medications, and surgical procedures, depending on severity and underlying cause.
Conservative Management
Physiological (normal) phimosis in young boys often resolves with age and rarely requires intervention.
Gentle daily stretching by retracting the foreskin as far as is comfortable may help but should be done cautiously to prevent trauma or paraphimosis.
Topical Treatments
Topical corticosteroid creams (such as betamethasone 0.05%, hydrocortisone 2.5%) applied to the tight ring of foreskin twice daily for 4 - 8 weeks can be effective for most cases of pathological phimosis by helping to soften and stretch the foreskin. Combined with gentle manual stretching this can be very effective.
Topical antibiotics may be prescribed if infection is present.
Surgical Procedures
Circumcision (complete removal of the foreskin) is the definitive treatment if conservative methods fail or phimosis is severe, recurrent, or associated with complications.
Preputioplasty (foreskin-preserving surgery) or a dorsal slit procedure may be considered in select cases, especially if only the tip is affected or preservation of foreskin is desired.
Treatment should always be tailored to age, symptoms, and family preference, with surgical options usually reserved for cases not responsive to medical management or where severe symptoms are present.
Circumcision on the Gold Coast
For some families, circumcision is pursued for medical, cultural, religious, or cosmetic reasons, or to address persistent foreskin problems. In my Gold Coast clinic, children circumcision is performed using the Plastibell technique - a gentle, safe option designed for infants and boys, with rapid recovery and minimal discomfort. Most children return to their regular routines with ease and parents receive ongoing support. Adult and teen circumcision options are available elsewhere, with experienced surgeons, using tailored surgical approaches suited to each age group.
Why Choose Circumcision at Medical on Robina?
As a GP who performs circumcisions here, I offer:
Years of experience in infant and child circumcision
Gold Coast-based service, no referral required
Compassionate advice about foreskin problems, development, and safe surgery
Experience with the Plastibell method for children
Book a Paediatric Circumcision Consultation
If you have questions about circumcision, foreskin care, or your child’s development - or if you want to book a circumcision procedure in the Gold Coast area - contact my clinic for friendly, expert advice and support.
For more information and appointments, reach out today.
Book a Consultation with Dr Carly Hupfeld
Whether you're ready to book or just want to learn more, we’re here to help you make the best decision for your family.
Dr Carly Hupfeld assess and manages oral ties and performs circumcisions:
Medical On Robina
T3/299 Scottsdale Dr, Robina QLD 4226
(07) 5690 1290
Could It Be a Tongue Tie? A Doctor’s Perspective on What to Look Out For
As an tongue tie doctor on the Gold Coast, spotting the signs of tongue tie early can make a dramatic difference in an infant’s feeding, maternal and infant comfort, and long-term oral development. A tongue tie isn’t always obvious, but knowing what to look for means parents can seek timely support and improve feeding, dental health, and speech outcomes.
What Is Tongue Tie?
Tongue tie (ankyloglossia) is a condition where the thin tissue under the tongue, called the frenulum, restricts normal tongue movement. This can impact an infant’s ability to breastfeed, bottle feed, and swallow. It can affect palate formation, dental alignment, and later, speech development.
Recognising tongue tie early makes a huge difference for both parents and babies and their feeding journey.
Physical Signs of Tongue Tie
Look for:
A tongue that can’t extend past the lips or appears ‘heart-shaped’ or notched at the tip when extended.
Difficulty lifting the tongue or moving it side to side.
Dimpling or cupping of the tongue.
A visible or tight frenulum under the tongue.
A white milk coating over the tongue (often misdiagnosed as thrush).
Tongue down or V-shaped when crying.
Functional Signs of Tongue Tie
Look for:
Feeding difficulties such as trouble latching or frequent slipping off the breast or bottle.
Poor weight gain or failure to thrive.
Fussiness or unsettled babies.
Windiness, colic or reflux symptoms.
Long feeds that never seem to satisfy.
Short feeds that never seem to satisfy.
Choking or gagging when swallowing.
Sleeping with mouth open and tongue down.
Inability to maintain suction on a dummy.
Persistent nipple pain, blocked ducts, or mastitis in mothers.
Misshaped nipples after a feed.
Tongue Tie Signs in Older Children and Adults
While most cases are detected in infancy, tongue tie can also cause issues later in life.
Speech problems, especially trouble making “t,” “d,” “l,” “n,” and “th” sounds clearly.
Problems licking lips or eating ice cream
Difficulties playing wind instruments.
Difficulty with oral hygiene or dental health.
Teeth crowding, narrow jaw or high palate.
Open mouth posture, snoring, headaches, or jaw tension.
Why Early Diagnosis Matters
As a tongue tie doctor, addressing these signs early helps prevent ongoing feeding frustration and helps prevent speech-related challenges or palate and dental related challenges in the future. If any signs or breastfeeding concerns occur, parents shouldn’t hesitate to reach out for professional advice or a tongue tie assessment.
If you’re worried your child might have a tongue tie, contact a trusted oral tie clinic for assessment and expert support.
“A tongue-tie diagnosis should never be based on appearance alone - it requires evidence of restricted movement and functional feeding difficulty.”
This blog is intended for educational purposes and does not replace individualized medical advice. For further information or assessment, please consult your healthcare provider.
Book a Consultation with Dr Carly Hupfeld
Whether you're ready to book or just want to learn more, we’re here to help you make the best decision for your family.
Dr Carly Hupfeld assess and manages oral ties and performs circumcisions:
Medical On Robina
T3/299 Scottsdale Dr, Robina QLD 4226
(07) 5690 1290
What to Expect When Your Child Undergoes Circumcision on the Gold Coast: A GP’s Personal Guide for Parents
As a Gold Coast GP specialising in infant circumcision, my goal is for every parent to feel confident and well-supported throughout the entire journey. Deciding to circumcise your child is deeply personal and sometimes overwhelming. With so much conflicting information and opinion online, my mission is to provide clear, evidence-based support - empowering families to make informed choices that feel right for them.
Why I Use the Plastibel Technique
In my practice, I favour the Plastibel method - a procedure trusted by families and backed by international guidelines for its safety, comfort, and predictable healing. During surgery, a small ring is placed under the foreskin, gently tied, and left to separate naturally over 7–10 days for infants, or up to 2 weeks for older boys. Most babies and young boys are back to their normal routines almost immediately. For infants, I recommend cuddles and a feed right after the procedure. Older children can return to whatever activities feel comfortable, with no special restrictions.
Risks and Safety
Safety always comes first in my clinic. Circumcision is generally very safe, especially in experienced hands – like mine. The most common risks - mild swelling, minor bleeding, and a low chance of infection - are usually brief and easy to manage. Studies show a very low complication rate, especially when the procedure is completed in the first year of life. I’m also personally available and on-call for all my patients, so you’ll never be left to worry alone.
Pain Management: Expert Protocols and Clinical Evidence
Minimising pain is absolutely central to my practice. For the procedure, I use a proven two-step pain relief protocol: first, a gentle topical anaesthetic cream, followed by a small local anaesthetic injection, once the cream is effective, for extra comfort. Latest research confirms that this approach dramatically reduces pain both during and after the procedure. In my experience, older children tend to remain relaxed and comfortable throughout the procedure, often happily distracted by a device or screen - giving us confidence that any discomfort is minimal. For most children, little or no pain relief is needed after Plastibel circumcision, but I routinely recommend paracetamol if any mild discomfort arises.
What Happens on the Day
Families often ask what to expect on procedure day. I begin with a careful consultation - whether days before or on the day of the procedure – discussing the medical history, the reasons for circumcision, the pros and cons of circumcision, explaining the steps of the procedure, and answering any questions. I then perform a gentle examination to ensure the procedure is necessary or appropriate and apply the numbing cream. While we wait for the cream to take effect, parents can go have coffee or remain seated in our ample waiting area. Once numb, the actual circumcision procedure then takes less than 20 minutes, parents wait in the waiting room or feeding room until we are done. Babies will feed immediately after the circumcision procedure while I reiterate the aftercare, older boys will be part of the aftercare conversation. Most families are ready to leave my clinic within an hour or so, confident about home care and recovery.
Recovery and At-Home Care
The Plastibell ring falls off naturally within 1–2 weeks. I’ll show you exactly how to use petroleum jelly morning and night, and keep the area clean with daily saltwater rinses. Bathing, dressing, and playtime can continue as normal. Mild swelling, redness, bruising, and a slight odour are all expected while the wound is healing and the bell and foreskin are detaching; anything more concerning, such as significant pain, bleeding, or signs of infection should be reported to me promptly. Remember -I’m on call throughout your child’s recovery.
My Commitment to Families
Providing compassionate, evidence-based care is the heart of my work. I know that circumcision is not just a medical procedure, but an emotional decision for many families. My Gold Coast clinic is dedicated to supporting you - before, during, and after your circumcision procedure - with direct answers, attentive follow-up, and total accessibility for your peace of mind.
If you’re considering circumcision but still have questions, please explore the rest of my website, or reach out to book a consultation. I’m always happy to provide personalised advice, evidence-backed guidance, and friendly support at every step.
Book a Consultation with Dr Carly Hupfeld
Whether you're ready to book or just want to learn more, we’re here to help you make the best decision for your family.
Dr Carly Hupfeld specialises in circumcision and oral ties at:
Medical On Robina
T3/299 Scottsdale Dr, Robina QLD 4226
(07) 5690 1290
Guiding Families on the Gold Coast: Navigating Circumcision and Oral Tie Decisions with Compassion and Expertise
Personalized care and empathetic communication are at the heart of supporting parents who face the difficult decision to pursue circumcision or oral tie release for their children on the Gold Coast. As a general practitioner - and mother of three - deep empathy informs every step, recognizing both the medical and emotional challenges involved.
The Emotional Journey of Parents
The experience of choosing circumcision or oral tie release is filled with complex emotions: worry, uncertainty, and the responsibility of acting in the child’s best interest. Many parents grapple with a flood of information, sometimes conflicting, from healthcare providers, friends, and family. These decisions can provoke anxiety about pain, recovery, and long-term outcomes, as well as guilt or second-guessing afterward. Open conversations and supportive guidance are key to making families feel secure, respected, and understood throughout this process.
Patient Care: Creating a Safe, Reassuring Environment
Children require special consideration in medical settings. Careful planning, gentle approaches to surgery, and thorough aftercare are essential for minimizing distress and promoting healing. Most procedures - like circumcision or oral tie releases - are designed to be safe with quick recovery, the child can return home on the same day and can resume all their regular activities. Honest discussions about what to expect can reduce fear and foster trust, while collaboration with other Gold Coast health care providers such as lactation consultants, osteopaths, chiropractors, speech therapists, and paediatric specialists ensures comprehensive care. Teamwork helps address not only immediate concerns (like feeding or speech), but also the child’s overall wellbeing.
Communication: Empowering Parent Decision-Making
Clear, honest communication is the foundation of trust between families and healthcare providers. Parents want understandable explanations of medical conditions, procedure details, risks, benefits, and recovery plans. Compassion means listening carefully, providing timely answers, and respecting every question -no matter how small and that’s what I aim to provide.
For issues like oral ties, I take time to assess the whole picture in detail, drawing on not only my own expertise, but the expertise of other allied health professionals also. With circumcision, I provide a non-bias discussion about the pros and cons, outline everything from fasting instructions to pain management, post-care, and emotional follow-up, letting parents feel prepared and supported.
The Unique Perspective of a GP Mother
Having three children of my own has given me special insight into the real-life fears and hopes of parents facing these choices. Every child is different. Every parent’s worry is valid. I know what it’s like to weigh the pros and cons, read and be given conflicting advice, and wonder what’s truly best for a child. My commitment as a GP on the Gold Coast is to combine medical skill with the compassion of fellow parent - walking alongside families through every decision and recovery milestone.
Conclusion: Supporting Informed, Confident Parents
When making medical decisions for a child, every parent deserves respect, compassion, and practical support. I provide a circumcision and oral tie service on the Gold Coast that’s focused on expert care, strong interdisciplinary teamwork, and communication that truly empowers families. As both a general practitioner and a mother, my approach honours the emotional experience of parents and provides the expertise and guidance they need to do what’s best for their children.
Book a Consultation with Dr Carly Hupfeld
Whether you're ready to book or just want to learn more, we’re here to help you make the best decision for your family.
Dr Carly Hupfeld specialises in circumcision and oral ties at:
Medical On Robina
T3/299 Scottsdale Dr, Robina QLD 4226
(07) 5690 1290
How long does it take to see results after a Tongue Tie Release?
As a GP with a sole interest in oral ties and circumcisions, I see a great number of concerned and frustrated parents. When it comes to tongue ties and upper lip ties, one of the most common questions I’m asked is: “When will we see improvement after a tongue tie release?”
The answer depends on your child’s age, symptoms, and the kind of support they receive afterwards - but here’s what most families can expect:
Immediate Results
For many babies, especially those with breastfeeding difficulties due to an oral tie, changes can be seen straight away. Infants may latch more effectively, feed with less effort, and mothers often report a reduction in nipple pain during the first feed after the procedure.
Early Recovery (First Few Days)
Some babies are a little unsettled at first, with the strange sensation and while their tongue adjusts to new movements. Improvements in feeding, in these instances, typically develop over the first 1–2 weeks, as sucking, swallowing, and tongue coordination gradually strengthen.
Long-Term Outcomes
Over weeks to months, the benefits consolidate. Babies may gain weight more steadily, feeding becomes less stressful, and mums notice lasting comfort. For older children, a release can improve speech clarity, chewing, swallowing, and oral function - especially when paired with support like lactation consultants or speech therapy.
Every Child is Different
Results vary - some improvements are immediate, others unfold gradually. What’s important is that the release gives the tongue freedom to function properly, supported by therapy when needed, for long-term oral health and development.
If you’re considering a tongue tie or lip tie assessment for your child, or if you’re seeking a trusted GP who also provides circumcision services, I specialise in these procedures with a family-centred and professional approach.
Reference List
Buryk M, Bloom D, Shope T. Efficacy of neonatal release of ankyloglossia: a randomized trial. Pediatrics. 2011;128(2):280-288. Found at: Efficacy of neonatal release of ankyloglossia: a randomized trial - PubMed
O’Shea JE, Foster JP, O’Donnell CP, Breathnach D, Jacobs SE, Todd DA, Davis PG. Frenotomy for tongue-tie in newborn infants. Cochrane Database Syst Rev. 2017;3:CD011065. Found at: Frenotomy for tongue-tie in newborn infants - PubMed
Amir LH, James JP, Beatty J. Review of tongue-tie release at a tertiary maternity hospital. J Paediatr Child Health. 2005 May-Jun;41(5-6):243-245. Found at: Review of tongue-tie release at a tertiary maternity hospital - PubMed
Bhattad MS, Baliga MS, Kriplani R. Clinical Guidelines and Management of Ankyloglossia with 1-Year Followup: Report of 3 Cases. Case Rep Dent. 2013 Jan 29;2013:185803. Found at: Clinical Guidelines and Management of Ankyloglossia with 1-Year Followup: Report of 3 Cases - PMC
Walsh J, Tunkel D. Diagnosis and Treatment of Ankyloglossia in Newborns and Infants: A Review. JAMA Otolaryngol Head Neck Surg. 2017;143(10):1032-1039. Found at: Diagnosis and Treatment of Ankyloglossia in Newborns and Infants: A Review - PubMed
Book a Consultation with Dr Carly Hupfeld
Whether you're ready to book or just want to learn more, we’re here to help you make the best decision for your family.
Dr Carly Hupfeld specialises in circumcision and oral ties at:
Medical On Robina
T3/299 Scottsdale Dr, Robina QLD 4226
(07) 5690 1290
A Day in the Life: Surgical Assistant, Gold Coast Circumcision and Oral Tie GP & Mum of Three
Juggling a career as a procedural GP specialising in tongue ties and circumcisions and being a mum of three on the Gold Coast, means every day is an organised - sometimes chaotic- adventure. Here’s how a typical day unfolds, blending patient care, family, and a dash of endorphins.
Sunrise Starts & Family Hustle
Most mornings begin before the sun, lacing up for a run through the Hinterland to clear my mind, get my body moving and get a shot of energy. The ten minutes with weights is a must for that extra boost. The next phase? The kitchen bustle: making kids’ lunches, prepping breakfast for whoever’s awake, packing afternoon tea, and gathering changes of clothes for the day’s activities. At this stage, my wonderful husband often steps in -finishing what I haven’t - and taking charge of the all-important school drop..
Ready for Work: Clinic or Theatre
After a quick shower and prepping for work, I head to either theatre or my GP clinic.
On Theatre Days:
Arriving anywhere from 6:30 - 7:30am, the anticipation builds as I prepare for knife to skin. I love that first, thorough five-minute surgical scrub- it’s the cleanest you’ll ever feel! The anaesthetist sets the tone with a playlist, and from here, the day flows: assisting on everything from complex stage 4 endometriosis surgeries, cystectomies, hysterectomies to caesareans. I embrace every moment in theatre, learning from and collaborating with amazing surgeons, offering help wherever it’s needed, totally immersed in the rhythm of surgical excellence.On Clinic Days:
The focus shifts to oral ties and circumcisions.I spend the day evaluating oral function, supporting parents in navigating feeding issues, and determining whether a tongue or lip tie is the cause. If we suspect a tie, I offer to perform a release on the spot, and we reassess feeding straight after. Sometimes, the results are felt or seen immediately, - these are always my favourite cases – because nothing is more rewarding; other times, improvement continues over a few weeks - time tells all.
For circumcision consults, I ensure parents (and children, if they’re older) have the facts and understand the procedure, risks, and medical necessity before we proceed. After applying numbing cream, I see another patient while we wait for it to take effect, then once the patient is numb, I can take them to the procedure room to complete the procedure.
My goal is always compassionate, expert care and clear communication every step.
Mum Mode: Afternoon Adventures
As the medical workday wraps, I swap my GP hat for chauffeur, snack provider, and homework helper. I pick the kids up, ply them with snacks, and ferry them off to extra-curriculars. Car park clothing changes and multitasking homework sessions ensue: one child here, another there, squeezing in reading or finishing assignments with the third until it’s time to swap or head home.
Evening Chaos & Connection
Home is a hive of homework finishing, dinner making, and the famous multi-child bath negotiation - who goes first, who avoids hair washing, and who can brush their teeth without a million reminders. Despite the mayhem, we end every day snuggled together for a bedtime story and song - if I can stay awake!
Why It’s Worth It
Being a Gold Coast surgical assistant, performing circumcisions, releasing oral ties and living the mum life means rising early, scrubbing up, and caring for patients - and racing to nurture my own family. Every day is busy and unpredictable, but the moments of laughter, triumph, and connection - both in theatre and at home - are utterly worth it.
How hard is it being a parent? Navigating choices, judgment & misinformation
Being a parent, in those early days with your newborn, or as they grow into independent children, is incredibly challenging. There’s an overwhelming amount of information, countless decisions to make, and no shortage of opinions and judgments at every turn. As a Gold Coast GP with a special interest in circumcisions and oral/tongue tie releases, I hear from families daily who feel the weight of these pressures.
Judgment at Every Step
From the moment your baby is born, everyone has an opinion, and it makes you question, “Should I circumcise my son? Is it an act of loving care or, as some wrongly and harshly claim, “genital mutilation?” The reality is that circumcision, when done professionally and with true informed consent, is a safe, legal, and sometimes culturally meaningful and medically beneficial choice for families in the Gold Coast and around Australia. Equating a medical procedure done under strict ethical guidelines with harmful practices is both inaccurate and unnecessarily guilt-inducing.
The Struggle with Feeding: Is It Supposed To Be This Hard?
Many parents come to me exhausted, anxious, and - too often -ashamed because feeding their baby isn’t going smoothly. “Should feeding really be this hard?” or “Should it take this long?” they ask me. For some babies, struggles with breastfeeding or bottle-feeding are due to conditions like tongue ties or oral ties - problems that, sadly, often go unnoticed by well-meaning friends, family, or even medical professionals.
It’s heartbreaking to hear stories of mothers who have faced shame or blame for “not trying hard enough” with breastfeeding, when the real issue was something as simple and treatable as a tongue tie. Sometimes, no one has even bothered to look inside the child’s mouth or worse, someone has looked and falsely deemed there to be no tie without a proper assessment or experience. How is a parent supposed to know what they don’t know?
Stop Explaining, Start Listening
Parenting isn’t about explaining yourself to everyone who has an opinion - it’s about listening to your child, your instincts, and qualified, supportive professionals. There’s no one-size-fits-all approach. Feeding struggles, difficult nights, and tough decisions - like whether to pursue circumcision or seek help for a suspected tongue tie - are all normal challenges that parents face.
Get Advice You Can Trust
If you’re worried:
Should I circumcise my child?
Does my son need a circumcision?
Is circumcision painful?
Does my child have a tongue tie?
Does my child have a lip tie?
Should feeding be this hard?
Should feeding take this long?
Should breastfeeding be this painful?
Does this tie require intervention?
Reach out to a medical provider with experience in these areas. Here on the Gold Coast, my focus is on support, accurate diagnosis, and skilled procedures for tongue ties, oral ties, and circumcision - without judgment, shame, or misinformation.
Parents: You’re Doing Your Best
If you’re trying, if you’re doing your best, that is enough. Don’t let the noise, opinions, or old myths influence your journey. Seek support from those who see you, who listen, and who can offer clear answers grounded in experience and empathy - because parenthood is difficult enough already.
For families on the Gold Coast who have questions about circumcision or tongue ties, you’re not alone. Your concerns are valid, and you deserve compassion and clarity, not judgment.
Making the Right Choice for Your Child
Whether you're ready to book or just want to learn more, we’re here to help you make the best decision for your family. I’m here to provide:
Accurate, evidence-based information
Safe, caring, and comfortable procedures
Supportive consultation for families from all backgrounds
Book with me, Dr Carly Hupfeld Circumcision and Oral tie GP
Medical On Robina
T3/299 Scottsdale Dr, Robina QLD 4226
(07) 5690 1290
The Realities of Breastfeeding: Embracing Challenges, Support, and Seeking Help
Breastfeeding is often described as one of the most natural things a mother can do - but that doesn’t mean it’s always easy. As both a general practitioner with a special interest in oral ties and circumcisions and a mother of three, I’ve seen, both personally and professionally, the joys and challenges that come with feeding your baby.
Breaking the Myth of “Natural = Easy”
There’s a widespread belief that breastfeeding will come naturally to every mother and child. While for some it does, for many, it involves a steep learning curve. Sore nipples, latch issues, concerns about milk supply, and worries about baby’s weight gain are just a few of the common hurdles. For mothers whose babies have oral ties, such as tongue or lip ties, these challenges can be even greater -creating frustration, pain, and even feelings of guilt or inadequacy.
My Journey as a mother
With my first child, I encountered unexpected hurdles. Despite all my training and preparation, I struggled with painful feeds, a fussy latch, jaundice and phototherapy. For the first 12 weeks, nipple shields became my lifeline. They allowed me to keep breastfeeding when I was close to giving up. It wasn’t the experience I had envisioned, but, in time, things improved. We ended up enjoying a full 12 months of satisfying breastfeeding, filled with moments of connection and pride.
When my second child was born, I naively expected a repeat of the first experience - or at least to feel prepared for the same challenges. Instead, my son’s start to breastfeeding was even more complicated: he needed an oral tie (tongue tie) released. Until that was addressed, we faced pain, frustration, and endless feeding sessions. After the procedure, the difference was remarkable. Feeding became easier, and we finally found our rhythm together.
With my third baby, I braced myself for more problems, especially since she also had a tongue tie. Yet, to my surprise, feeding her came easily, and the tie did not interfere nearly as much as I’d anticipated. Each experience was unique: what was essential for one child wasn’t needed for another, and despite similarities, no two journeys were ever the same.
The Power of a Support Team
Support can make all the difference. It might come from your partner, family, friends, healthcare professionals, or online communities. Sometimes, it means sitting with another mother who simply listens. Other times, it means leaning on specialists -lactation consultants, midwives, child health nurses, osteopaths, chiropractors, speech pathologists, GPs, paediatricians or oral tie specialists- especially when a medical issue like an oral tie is suspected.
For mothers encountering breastfeeding challenges, early intervention and support can improve comfort and outcomes. As a GP with a special focus on oral ties and circumcision based on the Gold Coast, I’ve seen firsthand how addressing issues like oral ties or feeding positions can transform a frustrating experience into a fulfilling one.
You Don’t Have to Do It Alone
The most important message I'd like to share is that asking for help is a sign of strength, not weakness. Breastfeeding can be a tough journey, but with the right support, it’s one you don’t have to walk alone. Whether it’s your first baby or your third, every experience is different, and every challenge is valid.
In Honour of Breastfeeding Week
Let’s celebrate the resilience of mothers everywhere, acknowledge the real challenges of breastfeeding, and remember the lifesaving impact of supportive, knowledgeable care. If you or someone you know is facing difficulties, reach out - help is there, and you deserve every bit of support along your breastfeeding journey.
Don’t compare your journey to anyone else’s or feel pressured to live up to a certain “standard.” Support, flexibility, and seeking help when you need it make all the difference.
If you’re struggling with breastfeeding latch, technique, pain or suspect a tongue or lip tie in your baby, reaching out to someone with experience is the best way to start.
Supporting You on the Gold Coast
Whether you need feeding support, a tongue tie assessment, or a tongue tie release, you deserve support every step of the way.
Book a Consultation with Dr Carly Hupfeld
Whether you're ready to book or just want to learn more, we’re here to help you make the best decision for your family.
Dr Carly Hupfeld specialises in circumcision and oral ties at:
Medical On Robina
T3/299 Scottsdale Dr, Robina QLD 4226
(07) 5690 1290
Remember: There’s no one-size-fits-all approach to feeding your baby. Trust yourself, reach out when you need help, and honour your own story
The Truth about Pain and Plastibell Circumcision: A Clinical Perspective
Plastibell circumcision is one of the most trusted and commonly performed methods for the circumcision infants and young boys. As a GP with advanced expertise in circumcision and tongue-tie procedures, I am committed to delivering professional care that prioritizes safety, comfort, and the well-being of every child.
Is Plastibell Circumcision Painful?
While the idea of circumcision pain can be anxiety-provoking for parents, modern techniques prioritize your child’s comfort at every step and studies show that topical and local anaesthetic provide adequate pain relief.
In my procedures, topical anaesthesia is applied before a local anaesthesia to numb the area, making the Plastibell procedure well tolerated by most children.
In my experience, most babies and children experience only brief, mild discomfort, if any, as the local is administered and little to non throughout the procedure. I have had some infants so relaxed that they sleep through the entire process, while older boys are most often completely at ease -happily occupied with some screen time throughout.
Majority of children need little or no pain relief after the procedure displaying minimal discomfort and quickly returning to their normal selves. However, like most things, pain perception varies, and some children may fuss briefly or require simple analgesics.
What to Expect: Pain Management and Recovery
Before the procedure: The area is numbed with topical and injectable anaesthesia for comfort.
During the procedure: Careful, expert technique keeps pain minimal.
Afterward: Paracetamol may be used for mild discomfort, but ongoing pain is rare. Most families note a speedy recovery, with children settling the same day.
Complications and serious pain concerns are rare (less than 1%), especially in experienced hands.
Every Child’s Experience Is Unique
Children’s pain responses vary based on age, temperament, and previous experiences. Approaching the process with clear information and reassurance can help families feel prepared. With skilled care and effective anaesthetic protocols, Plastibell circumcision is designed to minimize your child’s discomfort and ensure a smooth recovery. Most families report a positive experience and rapid return to normal routines.
References
Akhavizadegan H, Ghorbani A. Investigating Normal and Abnormal Features of Plastibell Ring Circumcision: Case Report and Review of Evidence. J Urol Surg. 2025;12(2):63-67 20-2024.2024-8-2.pdf
Brady-Fryer B, et al. Cochrane Review (2004): Demonstrates local anesthesia is effective in minimizing circumcision pain.
Fein, J. A., Zempsky, W. T., Cravero, J. P., & Committee on Pediatric Emergency Medicine. (2020). Relief of pain and anxiety in pediatric patients in emergency medical systems: Clinical report from the American Academy of Pediatrics. Pediatrics, 146(3), PEDS20122536 1391..1405
Rossi, S., Buonocore, G., & Bellieni, C. V. (2020). Management of pain in newborn circumcision: A systematic review. European Journal of Pediatrics. 2020 Aug 3;180(1):13–20. Management of pain in newborn circumcision: a systematic review - PMC
Book a Consultation with Dr Carly Hupfeld
Whether you're looking for a Gold Coast circumcision clinic, ready to book or just want to learn more about the circumcision procedure or the potential health benefits of circumcisions, we’re here to offer personalised advice and help you make the best decision for your family.
Dr Carly Hupfeld is committed to providing the highest standard of care and up-to-date information for families and specialises in circumcision and oral ties at:
Medical On Robina
T3/299 Scottsdale Dr, Robina QLD 4226
pH: (07) 5690 1290
Why parents generally aren’t in the room during circumcision and oral tie procedures: A GP’s perspective
As a GP with a special interest in circumcision and oral tie (tongue and lip tie) procedures, one of the most common questions I receive from parents is: “Can I be in the room with my child during the procedure?” I understand that this request comes from a place of love and concern. However, there are important clinical reasons why we ask parents to remain outside during these minor surgical procedures. This approach is designed to ensure the safest and most effective outcome for your child.
Minimising Distractions for Optimal Care
The primary reason we ask parents to wait outside is to minimise distractions for the doctor and the clinical team. Performing circumcisions or oral tie releases requires intense focus, precision, and a calm environment. Even the most well-intentioned parent can inadvertently create distractions - whether through movement, conversation, or emotional reactions - which can affect the concentration of the clinician and the efficiency of the procedure.
“Having a parent present is a distraction for the doctor, and we minimise distractions to focus totally on ‘doing a good job’.”
Supporting Your Child Before and After
Parents play a critical role before and after the procedure. For circumcision, you may be involved in applying anaesthetic cream prior to the procedure, and your presence and comfort are essential immediately afterwards for feeding and settling your baby. For oral tie procedures, immediate post-operative feeding is encouraged to help with healing and comfort. Your soothing presence is invaluable once the procedure is complete so having you ready is very important.
Reducing Stress for Your Child, yourself and the medical team
Children, especially infants, are highly sensitive to their parents’ emotions. If a parent is anxious or distressed, the child may sense this and become more unsettled. By having parents wait outside, we can often complete the procedure more quickly and with less emotional stress for the child.
Being in the procedure room with your child can be very stressful for parents because witnessing your child’s discomfort, feeling powerless, and managing your own anxiety in an unfamiliar medical environment can be emotionally overwhelming. Many parents also feel pressure to stay calm and supportive, which can add to the stress and uncertainty of the situation.
Having parents in the procedure room can be stressful for medical staff because it increases the risk of distraction, slows down procedures, and adds pressure to perform under close observation. Staff may also need to manage parental emotions and unpredictable reactions, making the situation more complex and potentially disrupting standard workflow.
So your child doesn’t associate you with the procedure
To help ensure your child doesn’t associate you with the procedure, it’s important to be aware that, especially with very young children, some temporary negative associations can occur if your child feels frightened while you are present but unable to actively comfort them. While remaining calm is usually reassuring and beneficial for your child, we also want to minimize any chance of your child feeling upset with you afterward. Being sensitive to their emotions, providing gentle comfort, and reassuring them after the procedure can help strengthen your positive connection.
Ensuring a Safe and Controlled Environment
Medical procedures require a controlled environment to reduce the risk of complications and to ensure that all infection control and safety protocols are followed. Limiting the number of people in the room helps maintain this environment and allows the clinical team to work efficiently and safely.
Space Constraints
Procedure rooms are often quite small and need to be kept clear for medical staff and equipment, to move safely and efficiently
Institutional Policy
Some clinics have policies that restrict parental presence for certain procedures.
Medical Reasons
If a parent is unwell, pregnant or if the child’s medical condition is complex, parental presence may not be allowed for safety reasons
“Ultimately the main goal is to provide the safest and most effective care for the child”
Common Questions
Can I see my child immediately afterwards?
Absolutely. Parents are reunited with their child straight after the procedure to provide comfort, feed, and settle them.
What about consent?
Both parents (if available/applicable) should provide informed consent before any non-life saving procedure like circumcision. This ensures everyone understands the risks, benefits, and alternatives before proceeding.
The Takeaway
While it’s natural to want to be by your child’s side, our policy of having parents wait outside during circumcision and oral tie procedures is based on best clinical practice. It allows us to focus fully on your child’s safety and comfort and ensures the best possible outcome.
If you have further questions about the process or your role as a parent, please don’t hesitate to ask during your consultation. Your child’s safety and comfort are always our top priorities.
Book a Consultation with Dr Carly Hupfeld
Whether you are interested in circumcision or concerned about a possible tongue tie or lip tie, Dr Carly is here to discuss with and support you in making the best choices for your family.
Dr. Carly Hupfeld specialises in circumcision and the assessment and management of oral ties at:
Medical On Robina
T3/299 Scottsdale Dr, Robina QLD 4226
(07) 5690 1290
Reference List
Kain, Z. N., Mayes, L. C., Wang, S. M., Caramico, L. A., & Hofstadter, M. B. (1998). Parental Presence during Induction of Anesthesia versus Sedative Premedication: Which Intervention Is More Effective? Anesthesiology, 89(5), 1147–1156. https://doi.org/10.1097/00000542-199811000-00009
Tume, L. N., & Carter, B. (2012). Parental presence during invasive procedures in children: A European survey. Anaesthesia, 67(10), 1157–1162.
American Academy of Pediatrics Committee on Pediatric Emergency Medicine (2014). Family Presence During Pediatric Procedures. Pediatrics, 133(5), e1459–e1467. Family presence during paediatric resuscitation and invasive procedures: the parental experience: An integrative review: An integrative review - PubMed
McGraw, T., & Kendrick, A. (1998). Booked admissions for day care surgery: Parental presence during induction of anaesthesia. Paediatric Anaesthesia, 8, 405–408. Effect of parental presence on anxiety during induction of anaesthesia in children undergoing elective day case surgery | Annals of Pediatric Surgery | Full Text
Heidarzadeh, M., Atashzadeh-Shoorideh, F., Mehran, A., et al. (2016). The effect of parental presence during invasive procedures on anxiety and cooperation in children: a systematic review. Journal of Pediatric Nursing, 31(4), 370–377.
Common Causes of Breastfeeding Issues: Insights from a Tongue Tie Doctor
As a doctor with a special interest in tongue tie releases and circumcisions, I frequently encounter families struggling with breastfeeding. Understanding the underlying causes of breastfeeding difficulties is essential for effective support and intervention.
Here are the most common reasons breastfeeding can become challenging, and how timely recognition can make a difference for both mother and baby.
Incorrect Attachment or Latch
The most frequent cause of breastfeeding problems is poor positioning or latch. When a baby is not attached well to the breast, it often leads to nipple pain, ineffective milk transfer, and even nipple trauma. This can quickly spiral into low milk supply and unenjoyable feeding times if not addressed.
Mastitis and Blocked Ducts
Mastitis is inflammation of the breast, typically resulting from blocked milk ducts. Causes include missed feeds, poor drainage, tight clothing, or trauma. Symptoms range from breast pain and redness to swelling and flu-like symptoms.
Nipple and Breast Infections
Infections such as thrush (a fungal infection) or bacterial infections can cause pain, redness, and discomfort. If left untreated, these infections may lead to early weaning.
Nipple Vasospasm
Nipple vasospasm occurs when the blood vessels in the nipple constrict, often triggered by cold or a history of Raynaud’s phenomenon. This leads to intense pain, burning, or throbbing, sometimes so severe that mothers consider stopping breastfeeding. Keeping nipples warm and ensuring a good latch can help reduce symptoms.
Tongue Tie (Ankyloglossia) and Upper Lip Ties
A Tongue tie, (a short or tight frenulum under the tongue) or a lip tie, (a short or tight frenulum under the lip), can restrict the baby's tongue or lip movements, making it difficult to latch and feed effectively. This can result in nipple pain, poor milk transfer, and frustration for both mother and baby. While tongue tie and lip tie is a recognized cause of breastfeeding issues, it is important to have a thorough assessment, as not all feeding problems are due to tongue tie.
Engorgement or fast Flow
When breasts become overfull, they can be painful and/or make latching difficult. This sometimes leads to blocked ducts or mastitis if not managed promptly.
Low Milk Supply
Low supply may result from infrequent feeding, poor latch, or underlying maternal health issues. Early intervention is key to restoring supply.
Insufficient Glandular Tissue (IGT) or mammary hypoplasia
Insufficient Glandular Tissue (IGT), also known as mammary hypoplasia, refers to a condition where the breast does not develop enough milk-producing (glandular) tissue. This can occur during several developmental stages, including in utero, puberty, or pregnancy and can result in the inability to produce an adequate milk volume, regardless of correct breastfeeding management and frequent feeding.
Even with perfect technique and enough breastfeeding sessions, parents with IGT may not make enough milk to fully nourish their baby
Nipple Shape or Trauma
Flat, inverted nipples, or damaged nipples, can make breastfeeding more challenging. They can make it harder for babies to latch and breastfeed effectively, which may lead to issues like poor milk transfer, nipple pain, and low milk supply. With extra support and proper techniques, many breastfeeding challenges related to nipple shape or damage can often be overcome.
Other Contributing Factors
Exhaustion, emotional stress, and maternal health problems can also impact breastfeeding success. Fatigue and stress may disrupt the hormonal processes needed for milk production and let-down, while health issues like thyroid disease or postpartum depression can further hinder lactation and make feeding more challenging. Comprehensive support, proper rest, treatment of health conditions, and access to lactation professionals are crucial in helping mothers overcome these obstacles and establish successful breastfeeding.
Birth Trauma
Birth trauma can cause breastfeeding issues by making it physically painful for mothers to nurse, interfering with a baby’s ability to latch and feed, and causing separation that disrupts bonding and milk supply. Emotional stress or psychological trauma from a difficult birth can further hinder milk production and make breastfeeding emotionally challenging, leading to early cessation or ongoing difficulties.
Early recognition of these issues and seeking support from healthcare professionals - such as lactation consultants, osteopaths, chiropractors, speech pathologists or tongue tie specialists - can make a significant difference in breastfeeding outcomes. If you are experiencing persistent pain, difficulty with latch, or concerns about your baby’s feeding, don’t hesitate to reach out for professional guidance.
For further support, consult a lactation consultant or a healthcare professional experienced in breastfeeding challenges and tongue tie management.
Book a Consultation with Dr Carly Hupfeld
Whether your child has a tongue tie or lip tie, or you’re seeking an assessment, we’re here to support you in making the best choice for your family.
Dr. Carly Hupfeld specialises in circumcision and the assessment and management of oral ties at:
Medical On Robina
T3/299 Scottsdale Dr, Robina QLD 4226
(07) 5690 1290
Reference List
Pregnancy, Birth and Baby. Nipple vasospasm and breastfeeding. Australian Government. Found at Nipple vasospasm and breastfeeding - symptoms, causes, management | Pregnancy Birth and Baby
The Royal Women’s Hospital. Nipple vasospasm. Accessed July 15, 2025. Found at: Nipple vasospasm | The Royal Women's Hospital
Better Health Channel. Mastitis and other nipple and breast problems. Victorian State Government. Accessed July 15, 2025. Found at: Breastfeeding – mastitis and other nipple and breast problems | Better Health Channel
La Leche League International. Tongue and lip ties. Found at: Tongue and Lip Ties - La Leche League International
Cleveland Clinic. Tongue-tie (ankyloglossia): symptoms, causes & treatment. Found at: Tongue-Tie (Ankyloglossia) Symptoms, Causes & Treatment
Arbour MW, Kessler JL. Mammary hypoplasia: not every breast can produce sufficient milk. J Midwifery Womens Health. 2013;58(4):457-461. Found at: Mammary hypoplasia: not every breast can produce sufficient milk - PubMed
5 Reasons male circumcision is not genital mutilation.
As a GP specializing in circumcisions, it’s important to address the misconception that male circumcision is equivalent to genital mutilation.
Here are five key reasons, supported by medical evidence and ethical analysis, why male circumcision is not the same as genital mutilation:
1. Proven Medical Benefits
Male circumcision significantly reduces the risk of HIV and other sexually transmitted infections, including genital herpes and high-risk human papillomavirus (HPV).
Male circumcision lowers the risk of urinary tract infections, penile infections (Balantitis), foreskin infections (posthitis), or Balanoposthitis – infection or inflammation of both the glans and foreskin.
Male circumcision also decreases the risk penile cancer, prostate cancer and cervical cancer for the female partners.
Male circumcision can prevent conditions such as phimosis (a tightening of the foreskin) and Balantitis Xerotica Obliterans (BXO) (an inflammatory skin condition) and can actually be the treatment for these conditions.
These health benefits distinguish circumcision as a preventive medical procedure, not an act of mutilation.
2. Low Risk When Performed Medically
When conducted by a trained medical professional, circumcision is a safe procedure with a low complication rate.
The complications arising from a medically performed circumcision are generally minor.
The risks associated with non-medical or ritual procedures have a higher risk of complications and more likely to be sever in nature.
The low risk profile of circumcision supports its classification as a medical procedure rather than an act of mutilation.
3. Ethical and Legal Justification
Major medical and ethical reviews conclude that, when performed for medical, cultural, or religious reasons, male circumcision is not a violation of human rights or bodily integrity.
Genital mutilation is widely recognized as a practice rooted in control, discrimination, and the violation of fundamental human rights.
Ethically, circumcision is justified by the principle of beneficence: the benefits outweigh the harms.
4. Distinct from Female Genital Mutilation (FGM)
Unlike FGM, which removes functional tissue and has no health benefits, male circumcision removes the foreskin (non-essential tissue) and provides clear, evidence-based health advantages.
Leading health organizations and legal frameworks recognize this distinction, and equating the two is misleading and unsupported by medical evidence.
5. Parental Choice and Cultural Context
Parents have the legal and ethical right to make informed decisions about their child’s healthcare, including circumcision, especially when considering cultural or religious values.
The procedure is deeply rooted in many cultures and religions, and banning it could lead to unsafe practices outside the medical system.
“Infant male circumcision fulfills the principle of beneficence based on the established benefits of circumcision. The harms associated with infant male circumcisions compared with the significant benefits associated with it make infant male circumcision meet the non-maleficence principle.”
If you are looking for a male circumcision clinic or want to discuss the procedure or the potential health benefits of circumcision, please contact our clinic for personalized advice. We are committed to providing the highest standard of care and up-to-date information for families considering circumcision.
Reference List
Alkhenizan, A., & Elabd, K. (2016). Non-therapeutic infant male circumcision: Evidence, ethics, and international law. Found at Non-therapeutic infant male circumcision. Evidence, ethics, and international law perspectives - PubMed
Benatar, M., & Benatar, D. (2003). Between Prophylaxis and Child Abuse: The Ethics of Neonatal Male Circumcision. The American Journal of Bioethics, 3(2), 35–48. https://doi.org/10.1162/152651603766436216
Benatar, D., & Benatar, M. (2003). 3:2 Target Article authors respond to Commentators: How Not to Argue About Circumcision. The American Journal of Bioethics, 3(2), 1–9. https://doi.org/10.1162/152651603102387820
Friedman, B., et al. (2016). Pros and cons of circumcision: an evidence-based overview. International Journal of Infectious Diseases, 46, 60–65. Found at Pros and cons of circumcision: an evidence-based overview - PubMed
Healthy Male Australia. Circumcision: Benefits, risks & procedure. Found at Circumcision: Benefits, risks & procedure | Healthy Male
Healthdirect Australia. Circumcision. Found at Circumcision | healthdirect
Moses, S., Bailey, R. C., & Ronald, A. R. (1998). Male circumcision: assessment of health benefits and risks. Sexually Transmitted Infections, 74(5), 368–373. Found at Male circumcision: assessment of health benefits and risks - PubMed
Pintye, J., et al. (2019). Benefits of male circumcision for MSM: evidence for action. The Lancet Global Health, 7(4), e392–e393. Found it Benefits of male circumcision for MSM: evidence for action - The Lancet Global Health
Stuart Rennie, Adamson S Muula, Daniel Westreich (2006) Male circumcision and HIV prevention: ethical, medical and public health tradeoffs in low-income countries. BMJ Jounal of Medical Ethics. 33 (6) . Found at 357.full.pdf
Tobian, A. A. R., et al. (2011). The Medical Benefits of Male Circumcision. PLoS Medicine, 8(7), e1000413. Found at The Medical Benefits of Male Circumcision
World Health Organization (2007). Male circumcision: global trends and determinants of prevalence, safety and acceptability. Found at unaids.org/sites/default/files/media_asset/jc1360_male_circumcision_en_0.pdf
Does child circumcision decrease sensitivity or future sexual pleasure?
As a GP specializing in child circumcision and paediatric procedures, I frequently receive questions from parents about the long-term effects of circumcision on sensitivity and sexual pleasure. If you are searching for “infant circumcision near me,” “child circumcision clinic,” or “benefits and risks of circumcision for boys,” this article is designed to provide clear, evidence-based answers.
What Is Child Circumcision?
Child circumcision is a minor surgical procedure that removes the foreskin covering the head (glans) of the penis. Evidence says it is best performed in the first 12 months of life, (as recovery is more seamless), but can be done at any stage of life. Many parents seek infant circumcision for cultural, religious, or medical reasons, and want to understand the potential impact on their child’s future health and well-being.
Does Circumcision Affect Sensitivity?
Research on sensitivity after circumcision is mixed:
Some studies suggest that men circumcised as adults report slightly reduced penile sensitivity and changes in orgasm intensity. However, these findings may not directly apply to boys circumcised as infants, as the developing nervous system adapts over time.
Other research, including studies on men circumcised as infants, shows no significant difference in penile sensitivity or sexual satisfaction compared to those who are not circumcised. The foreskin is sensitive to light touch, but sexual pleasure involves multiple types of sensation and psychological factors.
Does Circumcision Affect Sexual Pleasure in Adulthood?
For parents searching “does circumcision affect sexual pleasure later in life?” or “circumcision long-term outcomes,” the evidence suggests:
No universal answer: Some men report decreased sensitivity, while others notice no change or even improvement, especially if circumcision resolves medical issues like phimosis or recurrent infections.
Most men are satisfied: Studies show that the majority of men circumcised as infants or children report normal sexual function and satisfaction as adults.
Key Points for Parents Considering Child Circumcision
Child circumcision is a safe and common procedure when performed by an experienced doctor in a dedicated clinic.
Long-term effects on sensitivity and sexual function are generally minimal, especially for boys circumcised as infants.
Individual experiences vary: Factors such as age at circumcision, reason for the procedure, and individual anatomy can influence outcomes.
If you are looking for a child circumcision clinic or want to discuss the benefits and risks of circumcision for boys, please contact our clinic for personalized advice. We are committed to providing the highest standard of care and up-to-date information for families considering circumcision.
References
Morris BJ, Krieger JN. Does male circumcision affect sexual function, sensitivity, or satisfaction? International Society for Sexual Medicine, 2013. Found at: Does male circumcision affect sexual function, sensitivity, or satisfaction?--a systematic review - PubMed
Fink KS, Carson CC, DeVellis RF. Adult Circumcision Outcomes Study: Effect on Erectile Function, Penile Sensitivity, Sexual Activity and Satisfaction. Journal of Urology, 2002. Found at: Adult circumcision outcomes study: effect on erectile function, penile sensitivity, sexual activity and satisfaction - PubMed
Bossio JA, Pukall CF, Steele SS. Circumcision does not reduce penile sensitivity, research finds. Queen’s University Gazette, 2016. Found at: Circumcision does not reduce penile sensitivity, research finds | Queen's Gazette
Bossio JA, Pukall CF, Steele SS. Examining Penile Sensitivity in Neonatally Circumcised and Intact Men Using Quantitative Sensory Testing. Journal of Urology, 2016. Found at: Examining Penile Sensitivity in Neonatally Circumcised and Intact Men Using Quantitative Sensory Testing | Journal of Urology
Tian Y, Liu W, Wang JZ, et al. Effects of circumcision on male sexual functions: a systematic review and meta-analysis. Asian Journal of Andrology, 2013. Found at: Effects of circumcision on male sexual functions: a systematic review and meta-analysis - PubMed
If you are searching for “child circumcision near me,” “infant circumcision clinic,” or “circumcision for boys,” I am here to help. Contact my rooms today to learn more about our safe, evidence-based approach to paediatric circumcision.
Oral ties explained: Types, symptoms and why early release matters”
As a GP specialising in oral tie releases, I often encounter questions about the various types of oral ties, what they are, what they look like, where they are and their impact. Understanding these can help parents seek timely treatment. Below you will find a very brief summary of the types of oral ties.
The Different Types of Oral Ties
1.Tongue Ties (Ankyloglossia)
Tongue tie occurs when the lingual frenulum - the tissue connecting the underside of the tongue to the floor of the mouth - is unusually short or tight, restricting tongue movement.
The classification varies depending on your source, but the commonly used Coryllos classification separates tongue ties into 4 types.
This classification helps in diagnosing and determining the severity of tongue-tie conditions, but it doesn’t reflect the severity of the symptoms. As such, a functional assessment is always necessary to complete the diagnosis.
Types 1 & 2 are considered the “classical” type of tongue ties but type 3 and 4 can cause just as significant symptoms but are commonly missed.
Table 1.1 – The Coryllos Classification of tongue ties
2. Lip Ties (maxillary labial frenulum attachments)
The labial frenulum connects the upper lip to the gum. When tight or thick, it can restrict lip movement, potentially causing breastfeeding difficulties, poor latch, or dental hygiene challenges.
The Kotlow lip tie classification is a widely used system for describing the severity and location of upper lip ties in infants and children. It is based on where the frenulum attaches to the gingival (gum) tissue, helping clinicians assess the potential impact on function.
Class I is rarely restrictive, Class II and III may affect feeding or oral hygiene, depending on tightness, while class IV is most restrictive and most likely to cause functional problems. However, although the classification system helps guide treatment decisions, it does not always indicate symptom severity, as some children may compensate well despite a higher class tie.
Table 2.1 The Kotlow lip tie classification
3. Cheek Ties (Buccal Ties)
Less common, buccal ties involve a mucosal attachment from the cheek to the gum, which may affect oral function and comfort. They are classified based on the membrane attachment site.
Class 1 – Mucosal Attachment
Class 2 – Gingival Attachment
Class 3 – Alveolar Ridge Attachment
Under normal circumstances, the buccal frenulum supports the structure of the cheeks and lips. The membrane extends to both sides of your mouth, but if it’s too tight, it has been said to restrict normal cheek movement, interfering with the feeding process.
Why Early Diagnosis and Treatment Matter
Oral ties can interfere with breastfeeding, speech development, dental health, and even posture or breathing. Early assessment by a trained professional ensures appropriate management - whether it is monitoring, feeding support, bodywork, frenotomy, or frenuloplasty - leading to better outcomes.
If you have concerns, I am happy to consult with you and your family to discuss the symptoms and help make a proper assessment and diagnosis. To arrange an appointment, please call Medical on Robina to discuss your concerns with me.
References
Messner, A. H., Lalakea, M. L., Aby, J., Macmahon, J., & Meara, J. G. (2000). Ankyloglossia: incidence and associated feeding difficulties. Archives of Otolaryngology–Head & Neck Surgery, 126(1), 36-39. https://doi.org/10.1001/archotol.126.1.36
Hogan, M., Westcott, C., & Griffiths, M. (2005). Tongue-tie and frenotomy in infants with breastfeeding problems: A prospective, randomized trial. Pediatrics, 116(3), e1–e7. Randomized, controlled trial of division of tongue‐tie in infants with feeding problems - Hogan - 2005 - Journal of Paediatrics and Child Health - Wiley Online Library
Geddes, D. T., Langton, D. B., Gollow, I., Jacobs, L. A., Hartmann, P. E., & Simmer, K. (2008). Frenulotomy for breastfeeding infants with ankyloglossia: effect on milk removal and sucking mechanism as imaged by ultrasound. Pediatrics, 122(1), e188-e194. https://doi.org/10.1542/peds.2007-2087
American Academy of Pediatrics. (2012). Clinical Report: Ankyloglossia (Tongue-tie) and Breastfeeding. Pediatrics, 129(6), e1572-e1578. https://doi.org/10.1542/peds.2011-3552
If you suspect an oral tie is affecting feeding or speech, consult a healthcare professional experienced in diagnosis and release procedures for personalised care.Srinivasan, A., Al Khoury, A., Puzhko, S., Dobrich, C., Stern, M., Mitnick, H., & Goldfarb, L. (2019). Frenotomy in infants with tongue-tie and breastfeeding problems. Journal of Human Lactation, 35(4), 706–712. https://doi.org/10.1177/0890334418816973
A GP’s guide: When your son may need a circumcision? Understanding the medical indications
As a GP specializing in circumcision procedures, I frequently encounter questions about the medical reasons for circumcision or people asking if they should have their son circumcised. This guide outlines the key indications, helping patients and families make informed decisions.
What Is Circumcision?
Circumcision is the surgical removal of the foreskin covering the head of the penis. While often performed for cultural or religious reasons, there are also well-established medical indications.
Medical Indications for Circumcision
Absolute Medical Reasons
Pathological Phimosis
Phimosis is the inability to retract the foreskin. When caused by scarring or chronic inflammation (such as lichen sclerosis or balanitis xerotica obliterans), circumcision may be necessary if topical treatments aren’t adequate.
Signs of pathological phimosis include:
Inability to retract the foreskin (note this can be normal in younger boys)
Ballooning or bulging of the foreskin during urination
Pain or discomfort during urination, erection, or sexual activity
Redness, swelling or soreness of the foreskin
Difficulty urinating where the tight foreskin may block the flow leading to a weak stream or inability to empty the bladder fully
Discharge or odour due
White ring or scar tissue may indicate lichen sclerosis or repeated infections.
If your son is experiencing any of these symptoms, then he may have phimosis and benefit from a circumcision.
Figure 1.1 Symptoms of Phimosis
Recurrent Balanitis or Balanoposthitis
Repeated infections or inflammation of the glans (balanitis) or foreskin (balanoposthitis) can be indications for circumcision if other treatments fail or if they are recurrent and impacting life.
Relative Medical Reasons
Recurrent Urinary Tract Infections (UTIs)
In boys with recurrent UTIs, especially those with underlying urological abnormalities, circumcision may be considered, and the latter case is often recommended.
Paraphimosis
This is an emergency where the retracted foreskin cannot be returned to its normal position. Circumcision may be needed if episodes recur or if reduction is unsuccessful.
Figure 1.2 Phimosis vs Paraphimosis
Penile or Preputial Neoplasms
Suspicious or cancerous lesions may require circumcision for diagnosis or treatment.
Prevention of Sexually Transmitted Infections (STIs)
There is evidence that circumcision reduces the risk of HIV transmission in high-prevalence areas, as well as HPV rates though the benefit is less clear in low-prevalence regions.
Non-Medical Reasons
Many circumcisions are also performed for cultural, religious, or personal reasons.
As a medical practitioner, it is important to ensure that parents or patients are fully informed about the risks and benefits, especially when the procedure is not medically indicated.
Why Choose a GP Specializing in Circumcision?
As a General Practitioner with specialized training and experience in circumcision procedures, I am dedicated to providing safe, evidence-based care. I ensure that all patients and families receive thorough information, appropriate pain management, and high-quality follow-up. Circumcision is a decision that should be made carefully, with a full discussion of the risks, benefits, and available alternatives.
Where circumcision is considered the best option, I offer the plastibell technique for boys up to 12 or 13 years of age (depending on their size). The procedure is performed in my consulting rooms, eliminating the need for anaesthesia, costly hospital fees, or lengthy waitlists.
If you are considering circumcision for your son, if you think your son requires a circumcision, or if your older son is requesting the procedure, I am happy to consult with you and your family to discuss the process, risks, benefits, and necessity. To arrange an appointment, please call Medical on Robina.
Table 1.1 Reasons for Circumcision Summary
Reference List
· USANZ Guidelines: How to Perform Circumcision on Infant Males. Available at: USANZ - Guidelines on how to Perform Circumcision on Infant Males
· NHS: Circumcision in Men – Medical Reasons. Available at: Circumcision in men - NHS
· USANZ: Quality and Safety Considerations. Available at: USANZ - Guidelines on how to Perform Circumcision on Infant Males
· Patient.info: Indications for Circumcision. Available at: Circumcision: Assessment and Complications | Doctor
· The Urology Place: Adult Circumcision Before and After Photos. Available at: San Antonio Urology | Board Certified | Experienced Doctors
· Wikimedia Commons: Circumcision Images. Available at: Category:Circumcision - Wikimedia Commons
· Medical aspects of male circumcision. BMJ. 2007 Dec 8;335 (7631): 1206 – 1209. Morris BJ, Wiswell TE. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC2128632/1
· Circumcision StatPearls. Treasure Island (FL): StatPearls Publishing; 2024.Stang HJ, Snellman LW. Available at: https://www.ncbi.nlm.nih.gov/books/NBK535436/2
· Male circumcision: Global Trends and Determinants of Prevalence, Safety and Acceptability. World Health Organization. 2007. Available at: https://apps.who.int?iris/bitstream/handle/10665/43749/9789241596169_eng.pdf
· Adult Circumcision. American Family Physician.1999 Mar 15;59(6):1514-1518. Weiss HA, Larke N, Halperin D, Schenker I. Available at: https://www.aafp.org/pubs/afp/issues/1999/0315/p1514.html
· Circumcision for phimosis and other medical indications in Western Australian boys. Med J Aust. 2003 Feb 17;178(4):155-8. Spilsbury K, Semmens JB, Wisniewski ZS, Holman CD. Available at: https://www.mja.com.au/system/files/issues/178_04_170203/spi10278_fm.pdf
· Circumcision. Raising Children Network. October 2024. Available at: https://raisingchildren.net.au/guides/a-z-health-reference/circumcsion
· Circumcision Clinical Presentation: Physical Examination. Medscape. Updated: Jan 31, 2020. Available at: https://emedicine.medscape.com/article/1015820-clinical
· Circumcision of Infant Males. Royal Australasian College of Physicians (RACP). Position Statement. 2010. Available at: racp-circumcision-of-infant-males-position-statement.pdf
Circumcision in infants and children: Weighing the benefits and risks
As a Gold Coast GP specialising in circumcision and tongue-tie releases, I’m often asked by parents about the benefits and risks of infant circumcision. With so much information, and misinformation, online - it’s essential to base decisions on the best available medical evidence and guidelines. Here’s what you need to know if you’re considering circumcision or tongue tie procedures for your child.
A circumcision is a surgical procedure that involves the removal of the foreskin, which is the fold of skin covering the tip (glans) of the penis. This procedure is often performed for medical, cultural, religious or personal reasons. In infants and children, circumcision is typically done under local anaesthesia by a trained medical professional in a sterile environment to minimise risks.
Figure 1: The Penis before and after circumcision
Circumcision in Infants and Children: What are the Benefits?
Reduced Risk of Infections
Urinary Tract Infections (UTIs): Circumcision lowers the risk of UTIs in infants, especially those with urinary tract or kidney abnormalities. The Association of American Physicians (AAP) reported that circumcised infants have a 10x lower risk of urinary tract infections in their first year.
Sexually Transmitted Infections (STIs): There is evidence that circumcised males have a reduced risk of acquiring HIV and certain other STIs, including HPV and herpes simplex virus. Some studies have shown a 50 -60% lower risk of HIV and HPV transmission in adulthood. However, these benefits are most relevant in regions with high STI prevalence, and this is far less pronounced in Australia.
Reduced Risk of Cancer
Penile Cancer: Circumcision is associated with a slightly lower risk of penile cancer, and the benefit has been shown to be most significant when circumcision is performed in infancy or childhood, before potential exposure to human papillomavirus (HPV) and other risk factors. However, this cancer is extremely rare in Australia and New Zealand, and the absolute reduction in risk is very small.
Prostate Cancer: Some studies suggest that circumcision may be linked to a lower risk of prostate cancer due to reduced risk of sexually transmitted infections that may contribute to prostate inflammation and subsequent cancer risk. However, again, the evidence for a protective effect against prostate cancer is less robust than for penile cancer, and the association is not considered strong enough to recommend circumcision solely for prostate cancer prevention
Prevention of Foreskin-Related Conditions
Circumcision can prevent conditions such as phimosis (tight foreskin), balanitis (inflammation of the glans) and recurrent infections. Over a lifetime, more than half of uncircumcised males may experience a foreskin-related issue.
Easier Hygiene
Removing the foreskin makes penile hygiene simpler, reducing the risk of smegma buildup and infections and irritation.
Risks and Considerations of Circumcision
Surgical Risks
Complications are rare when performed by experienced professionals, but can include bleeding, infection, scarring (1–2% of cases, usually minor), and very rarely, injury to the penis (<0.1% risk).
Pain and Recovery
While the procedure is generally quick, pain management is important.
Topical anaesthesia is used prior to local anaesthesia to minimise discomfort during the procedure
Post operatively, most infants recover within 7–10 days while older boys can take up to 2 weeks and simple analgesia is usually more than adequate.
Ethical and Cultural Considerations
Infant circumcision involves important ethical considerations because it is a non-therapeutic procedure performed on babies who cannot consent, and it permanently removes tissue.
While the procedure is generally safe and may offer some health benefits, as discussed, it also carries risks and raises questions about respecting the child’s future autonomy and bodily integrity.
What do Medical Organisations say?
Most medical organisations agree the health benefits slightly outweigh the risks, but not enough to recommend routine circumcision for all newborns.
The Royal Australasian College of Physicians (RACP) reviewed the current evidence and found that while circumcision is generally safe, the frequency of diseases it can prevent is low in Australia and New Zealand. Therefore, the RACP does not recommend routine infant circumcision for healthy boys, stating that “the benefits do not clearly outweigh the risks”. They acknowledge there are clear benefits in certain circumstances – for instance, for infants with significant urinary tract abnormalities or recurrent infections.
The RACP supports parental choice provided:
The procedure is performed by a qualified, experienced practitioner.
Accurate, unbiased information about risks and benefits is provided.
Appropriate anaesthesia and a child-friendly environment are ensured for safety.
The Urological Society of Australia and New Zealand (USANZ), and other bodies support the RACP statement, emphasising that the risks of non-medical circumcision generally outweigh the benefits for well infants.
Conclusion
Circumcision is a safe and effective procedure with well-documented benefits for certain medical conditions. However, for most healthy infants in Australia, the risks and ethical considerations mean routine circumcision is not universally recommended. The decision is personal - parents should weigh the evidence, consider their values and consult with a trusted, experienced GP.
If you have questions about circumcision or tongue-tie procedures for your infant or child, I am located on the Gold Coast at Medical On Robina and you can book a consultation for expert, compassionate advice.
Circumcision and Tongue Tie Services on the Gold Coast
As a GP with a focus on circumcision and tongue-tie releases, I provide:
Evidence-based advice tailored to your child’s needs and your family’s values.
Safe, gentle procedures using the latest techniques and pain management protocols.
Comprehensive aftercare to ensure the best outcomes for your child.
Frequently Asked Questions
Is circumcision covered by Medicare?
In Australia, circumcision is only covered by Medicare if medically necessary (e.g., for recurrent infections or phimosis).Are there alternatives to circumcision?
Yes - good hygiene, safe sexual practices and regular medical checkups can prevent most foreskin-related issues in uncircumcised boys.What about tongue ties?
Tongue-tie (ankyloglossia) can affect feeding, speech and oral health. If you have concerns about your child’s tongue movement or feeding, an assessment by an experienced provider can determine if a release may be appropriate.
Resources and Further Reading
PubMed. “Pros and cons of circumcision: an evidence-based overview.” Pros and cons of circumcision: an evidence-based overview - PubMed
University of Sydney. (2017, February 8). Male infant circumcision has a 200 to one risk-benefit: research. University of Sydney News. Male infant circumcision has a 200 to one risk-benefit: research - The University of Sydney
Raising Children Network. (n.d.). Circumcision. Retrieved from https://raisingchildren.net.au/guides/a-z-health-reference/circumcision
Moses, S., Bailey, R. C., & Ronald, A. R. (1998). Male circumcision: assessment of health benefits and risks. Sexually Transmitted Infections, 74(5), 368–373. https://doi.org/10.1136/sti.74.5.368
Morris, B. J., Bailis, S. A., & Wiswell, T. E. (2017). Early infant male circumcision: Systematic review, risk-benefit analysis, and progress in policy. World Journal of Clinical Pediatrics, 6(1), 89–102. https://doi.org/10.5409/wjcp.v6.i1.89**
Royal Australasian College of Physicians. (2022). Circumcision of infant males [PDF]. Royal Australasian College of Physicians. https://www.racp.edu.au/docs/default-source/advocacy-library/racp-circumcision-of-infant-males-position-statement.pdf?sfvrsn=92edd11a_4
Urological Society of Australia and New Zealand. (n.d.). Guidelines on how to perform circumcision on infant males. Urological Society of Australia and New Zealand. https://www.usanz.org.au/info-resources/position-statements-guidelines
Urological Society of Australia and New Zealand. (n.d.). RACP position statement on circumcision of infant males. Urological Society of Australia and New Zealand. https://www.usanz.org.au/info-resources/position-statements-guidelines
Nature. (n.d.). Royal Australasian College of Physicians' recent policy on infant circumcision. Nature. https://www.nature.com/articles/s41390-024-03190-8.pdf
Pediatric Research. “Detrimental to public health: Royal Australasian College of Physicians’ recent policy on infant circumcision.” https://www.nature.com/articles/s41390-024-03190-8.pdf
RACP. Circumcision – Parent information. circumcision-brochure-2024.pdf
RACP. Policy and Advocacy Library. https://www.racp.edu.au/policy-and-advocacy/search#:~:text=The%20RACP%20submission%20refers%20to%20specific%20proposals%20for,Policy%20and%20Advocacy%20Library%20for%20published%20policy%20documents.
World Journal of Clinical Pediatrics. “Early infant male circumcision: Systematic
Mayo Foundation for Medical Education and Research. (2024). Circumcision: What you can expect. Mayo Clinic. https://www.mayoclinic.org/tests-procedures/circumcision/about/pac-20393550
Keywords: Circumcision Gold Coast, Infant circumcision, Child circumcision, Paediatric circumcision, Circumcision risks, Circumcision benefits, RACP circumcision guidelines, Circumcision clinic Gold Coast, Tongue tie Gold Coast, Tongue tie release,
Understanding Tongue Tie (Ankyloglossia): A Comprehensive Guide for Parents and Healthcare Professionals
Tongue tie, medically known as ankyloglossia, is a condition that has generated significant discussion in both clinical and parenting circles. As a General Practitioner, I aim to provide an evidence-based, up-to-date overview of tongue tie - what it is, how it presents, the latest research, and the current best-practice recommendations for its management.
Tongue tie occurs when the thin band of tissue connecting the underside of the tongue to the floor of the mouth (the lingual frenulum) is unusually short, thick, or tight. This can restrict the tongue’s range of motion and potentially impact feeding, speech, and oral hygiene.
Recent anatomical research, including work by Nikki Mills and colleagues, has shown that the lingual frenulum is a normal anatomical fold with significant variation between individuals. Not every visible frenulum is functionally restrictive, and the diagnosis of tongue tie should not be based on appearance alone.
Symptoms and Signs of Tongue Tie
Tongue tie can present with a spectrum of symptoms, most commonly in infants who are breastfeeding. Key symptoms and signs include:
Breastfeeding difficulties: Poor latch, prolonged feeds, poor milk transfer, clicking sounds, or the infant slipping off the breast, frustrated feeds, and frequent feeds.
Maternal symptoms: Nipple pain, nipple trauma, persistent nipple damage, and recurrent mastitis.
Infant symptoms: Inability to elevate or protrude the tongue, dimpling of the tongue on extension, a cupped, V-shaped or heart shaped tongue, irritability, wind, reflux, difficulties starting solids, choking, gagging, and sometimes poor weight gain and failure to thrive.
Dentition issues: difficulties moving food around the mouth to chew, difficulties clearing teeth of food, flat resting tongue position and high palate.
Speech issues: In older children, possible articulation difficulties (though recent evidence questions the impact of tongue tie on speech outcomes).
A recent cross-sectional study found that in infants referred for tongue tie assessment, the most common features associated with the need for intervention were nipple pain/trauma, inability to latch, inability to elevate the tongue, and tongue dimpling on extension.
How Is Tongue Tie Diagnosed?
Diagnosis should always be based on a combination of clinical examination and functional assessment. Major guidelines and best-practice recommendations emphasize:
Assessment of tongue movement and function: Not just the appearance of the frenulum.
Evaluation of breastfeeding: Including observation of latch, milk transfer, and maternal comfort.
Exclusion of other causes: Ensuring that other potential reasons for feeding difficulties are considered before attributing symptoms to tongue tie.
Tools such as the Hazelbaker Assessment Tool for Lingual Frenulum Function (HATLFF) are sometimes used to standardize assessment.
Current Evidence: What Does the Latest Research Say?
Breastfeeding and Tongue Tie
Ultrasound studies have shown that effective milk transfer is more dependent on the intra-oral vacuum created by the baby’s jaw and tongue, rather than just tongue movement. Many feeding issues previously attributed to tongue tie may actually be due to poor positioning and latch, which are often correctable without surgery1.
Surgical release (frenotomy) has shown to improve breast feeding effectiveness, reduce nipple pian, increase maternal self-efficacy and reduce gastro-oesophageal reflux disease.
Treatment Options for Tongue Tie
Conservative (Non-Surgical) Management
First-line approach: For most infants, non-surgical strategies are recommended initially. These include:
Optimizing breastfeeding technique (positioning and latch)
Lactation consultant support
Speech pathology support
Bodywork with an orofacial myologist, osteopath, chiropractor, or paediatric physiotherapist
Addressing milk supply issues with pumping or medications such as motilium.
Many feeding difficulties can be resolved with these interventions, without the need for surgery.
Surgical Management: Frenotomy
Indication: Frenotomy should only be considered when there is a clearly defined structural restriction causing persistent functional feeding difficulty, and when conservative measures have failed.
Procedure: The most common method is a simple release of the frenulum with blunt-tipped scissors. Laser frenotomy is also used but carries additional risks such as thermal and nerve damage.
Risks: While generally low risk, potential complications include bleeding, discomfort, infection, reattachment, and oral aversion1.
Post-Operative Care
Immediate breastfeeding support is recommended after the procedure to maximize the chances of successful feeding and minimize complications15.
Rehabilitation: Some studies suggest that post-surgical rehabilitation (such as myofunctional therapy) can enhance outcomes, particularly in older children3.
Best-Practice Recommendations
Based on the latest evidence and guidelines from organizations such as the Academy of Breastfeeding Medicine, Speech Pathology Australia, and the Australian Dental Association, the following approach is recommended:
Assess function, not just appearance.
Try conservative management first.
Reserve surgery for clear, persistent functional problems.
Use scissors rather than laser for infants.
Provide comprehensive breastfeeding support post-procedure.
Avoid unnecessary release of lip or cheek ties.
Key Takeaways for Parents and Healthcare Professionals
Tongue tie is common, but not all cases require intervention.
Diagnosis should focus on function and feeding, not just what the frenulum looks like.
Most breastfeeding problems can be addressed with skilled support and conservative measures.
Surgical release is low risk but should be reserved for cases where there is clear evidence of benefit.
Recent References and Further Reading
· Douglas, P., & Geddes, D. (2018). Ultrasound imaging of tongue function in breastfeeding. Midwifery, 62, 1–8
· Mills, N., Pransky, S. M., Geddes, D. T., & Mirjalili, S. A. (2019). Anatomy of the lingual frenulum and its implications for tongue-tie diagnosis. Clinical Anatomy, 32(7), 1025–1032
· Melong, C., Smith, A., & Johnson, L. (2024). Speech outcomes following tongue-tie (ankyloglossia) release in children: A prospective study. International Journal of Pediatric Otorhinolaryngology, 174, 111234
· Ferrés-Amat, E., Pastor-Vera, T., Rodriguez-Alessi, P., Ferrés-Amat, E., Mareque-Bueno, S., & Ferrés-Padró, E. (2022). Outcomes of tongue-tie release and myofunctional therapy: A systematic review. Journal of Clinical Medicine, 11(4), 1022.
· S mith, J., Lee, A., & Patel, R. (2024). Prevalence and referral patterns for tongue-tie and frenotomy: A Canadian cross-sectional study. Canadian Journal of Paediatrics, 29(2), 85–92
· Royal Hospital for Women (NSW Health). (2019, reviewed 2024). Tongue Tie Assesment and Management Guidlines. Sydney: NSW Health
· Cordray, H., Raol, N. P., Mahendran, G. N., Tey, C. S., Nemeth, J., Sutcliffe, A., Ingram, J., & Sharp, W. G. (2024). Quantitative impact of frenotomy on breastfeeding: A systematic review and meta-analysis. Pediatric Research, 95(1), 34–42.
· Bruney, T. L., O'Shea, J. E., & Watson, J. (2022). Systematic review of the evidence for resolution of common breastfeeding problems—Ankyloglossia (Tongue Tie). Acta Paediatica, 111(5), 1007–1015.
Conclusion
Tongue tie is a nuanced condition that requires careful assessment and a balanced, evidence-based approach. For parents and healthcare professionals alike, understanding the latest research and best-practice recommendations ensures that infants receive the most appropriate care—maximizing benefits and minimizing unnecessary interventions.
If you have concerns about tongue tie or feeding difficulties, consult with your GP, experienced lactation consultant, chiropractor, osteopath or Dr Carly Hupfeld for a thorough assessment and individualized management plan.
“A tongue-tie diagnosis should never be based on appearance alone—it requires evidence of restricted movement and functional feeding difficulty.”
This blog is intended for educational purposes and does not replace individualized medical advice. For further information or assessment, please consult your healthcare provider.
Book a Consultation with Dr Carly Hupfeld
Whether you're ready to book or just want to learn more, we’re here to help you make the best decision for your family.
Dr Carly Hupfeld assess and manages oral ties and performs circumcisions:
Medical On Robina
T3/299 Scottsdale Dr, Robina QLD 4226
(07) 5690 1290